Shanksteps Bere 2024
We are back in Bere, Chad. It is the HOT season. Our room is about 95 to 97deg F in the
evening. Im able to fall asleep for about 2 hours then Im awake again, hot and jetlagged. I lay
there till morning. I get up and all I want is cold water. It’s a choice. We have a refridgerator in
the place we’re staying, but the more water or things we put in it the hotter the room it’s in
gets, as expected. So its a tradeoff. Denae and Steven are doing a very difficult surgery in the
morning before she leaves. It’s a enterocutaneous fistulae (connection of the intestine to the
abdominal wall that makes stool to leak out a hole onto the belly). As they work on that I go
and make rounds. Emma, the surgical ward nurse, is knowledgeable about their different
reasons for surgery and rounds go fairly quickly. I look at all the wounds that are granulating
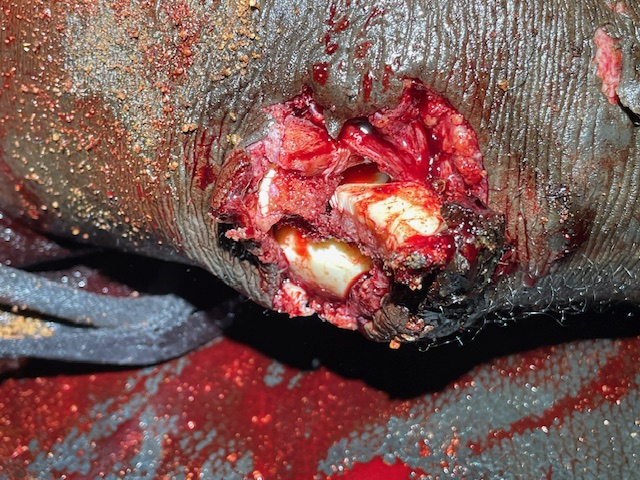
and change the dressings. One dressing stands out: This guy of about thirty has seizures and
during a seizure fell in the fire and burned his foot and head. I have yet to ask him what
contortion allowed this to occur! But he came in a couple weeks ago with three toes burned
and his head charred. After taking off his dressings i see that the three toes are super floppy,
almost like they don’t have any bones in them?? One has a bone because it is sticking out the
end of his toe. As I take off his scalp dressing I see that he has good granulation around the
outside and a patch of about 2x4inches of exposed skull. I know that skin grafting doesn’t
work on a bone, so this will need special attention. I see the patients with vessicovaginal
fistulaes that Dr. Denae has operated on and they are in various stages of their 4 weeks with a
urine catheter. Some have been “discharged” to the outside to save bed space for other
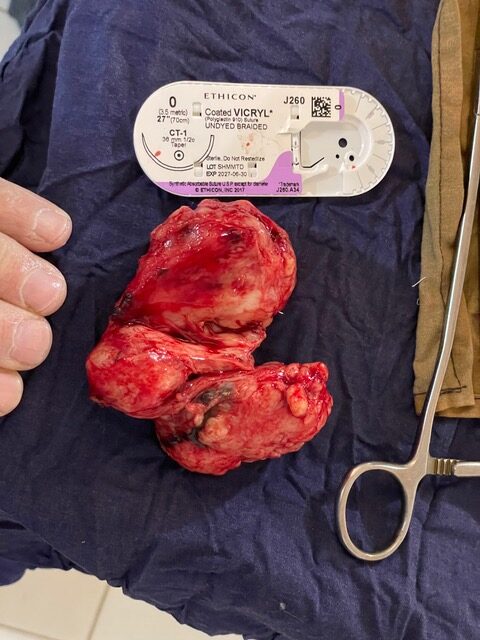
patients, and they come in to be seen while rounds are made. others have had hystorectomy,
hernia repair, hydrocele- that ended up being a hernia stuck to a testicle and they had to take
the testicle (orchiectomy). I see a boy with a humerus fracture that he got climbing in a tree
and falling out of it. Thats how most of the children break bones, climbing in a mango tree to
get mangos and falling to the ground.
I head back to “my” house, which by the way is the place I’ve stayed in before. I think it’s the
place James and Sarah Appel first built when they started building stuff in Bere. I unpack
some things and then go and check how things are going in the OR. i do some other surgery –
which i don’t remember now. Then we get done earlier since its a Friday and we like to be out
for Sabbath if possible. We really value Sabbath rest as Jesus observed it. Im able to visit with
old friends (missionaries) and it’s a nice evening.
Im called in to see 4 accident patients. The nurse says one has an open knee and the others
with broken arms, but not open. They were on motorcycles that hit one another. I remember
that most patients once they’ve been diagnosed with a fracture, want to be treated by the
traditional bone healer. So i tell him, whoever wants me to treat them, have them stay. if they
want the bone healer they can go. So when i get in there to see them, only the guy with the
open knee fracture is left. So I look and all is see is pieces of his patella (knee cap) sticking out
at odd angles. As i touch it pieces come off in my hand. Dirt and sand is everywhere. I ask for
an X-ray, but the nurse tells me the person lives to far away and phones are not working. So i
tell them to send someone to get him and someone to get the OR crew of Philipe and David.
Only David comes in. But the guy who does the sterilization of instruments says he can help.
So I go to the OR after waiting about .1.5 hours to get ahold of the right people without
success. In the OR i help the assistant gown up as I don’t think he really knows about sterility.
Not that this knee is sterile- it has dirt and sand in it. I find there is no identifiable knee cap. i
see a piece of the end of the femur chipped off and no other identifiable structures. I open it
up more and more and still cant identify any remaining structures. So i wash it out and close
the skin and plan on an Xray tomorrow. To see if that gives me any more clarity as to what can
be done. I head home.
i shower and get into bed dripping wet. I sleep for maybe an hour then lay awake most of the
night tossing and turning. it’s still hot!!(In the next day or so, i am informed in the operating room that this guy wants to go home. And
he signs out against medical advise)