Bere 5/2025 #8
Sabbath was a peaceful day. Dr. Andrew took his kids to the “monkey forest” and they saw monkeys pretty close early in the morning. I had a peaceful morning and then rode the big motorcycle to church with Zach on the back. I went to the same church as last week. It was unbearably hot with rain clouds all around but no rain at potluck. Some people went to the river again and that was what I was hoping would happen. I was cooler than the air and lovely to lay in the shallow brown cow poop shistosoma filled water. In the evening I hung out with some missionaries and talked.
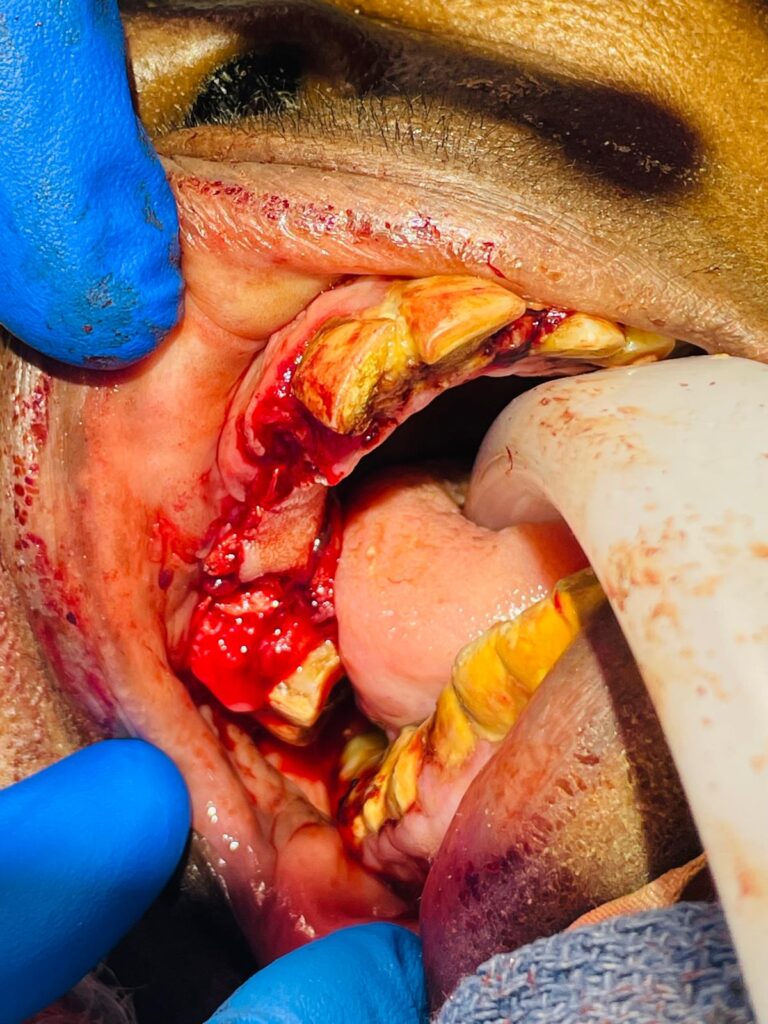
Sunday AM I am awakened about 5AM for a woman who has had 5 babies and all of them died during labor. Her last one ruptured the uterus. This one doesn’t seem to be progressing. So I go in thinking she likely needs a C-section. This nurse I remember I haven’t had much confidence in, in the past. I see that the babies head doesn’t descend much during a contraction and I ultrasound the baby. As I watch another contraction I see the heart rate slow down and it stays slow after the contraction. Fetal distress. I call in the team for an emergent C-section. The maternity nurse brings the patient to the OR and we get her ready as Phillipe gets there. It seems to move along faster than normal. She has a previous scar on her lower abdomen from the uterus repair before. It seems like a keloid (thick and large and hard), so I excise the previous scar. Her scar tissue is pretty dense. After opening the muscles I find the bladder quite stuck and I can’t even drop it down out of the way. I imagine this is because of the previous site of rupture and scaring. So I have to make a higher transverse incision on the uterus than normal. I reach into the uterus to grab babies head and it is wedged into the pelvis. I work my fingers hard to try to get around the head to pull it back up. It’s real hard to get my fingers around it then the suction of the pelvis holds my hand there, finally a bit of air goes around my hand and the suction is broken and Im able to pull up the head. The baby is floppy. And since I don’t trust the nurse I keep the baby on the wound in front of me for a little bit and get him breathing before handing him off to her. The closure of the abdomen is uneventful and after about 5 minutes her and the anesthetist working on the baby, he’s breathing well.
The next patient we are suppose to do is a liver abscess but the power went out again. This time I think they’re filling the generator. They have two new generators that they say have oil cut off sensors that are bad?? Unlikely on a new generator. More likely poor oil amount or quality. So since I don’t have power I go to make rounds. I take my headlamp and see all my patients in about an hour.
I go back to the OR and about then the power comes back on. So they bring the patient in and I decide to ultrasound his liver to decide whether I’ll do it with a pigtail drain or open drainage. There is no abscess. I check the paperwork and it says a bladder stone on the ultrasound. Is this the patient in bed 9 with the abscess? Yes. The anesthetist steps out to find out more. They come back with the correct patient who’s been out under a tree so some other patient took that bed. Ultrasounding the correct patient, I see there is a deep abscess in the posterior liver up near the diaphragm and heart. OOOhhh. If I miss the direction I could stab the heart and kill him. I think about not draining it. But it won’t get better without drainage and in the posterior liver, draining it with open surgery will be nearly impossible too. So decide to put in a spinal needle in the direction I think I should go and watch on ultrasound. I get right into it. So I take the much larger pigtail catheter and feed it in till I see the tip in the middle of the abscess. I withdraw about 80ml of pus. I flush it with saline and attach a bulb for suction.
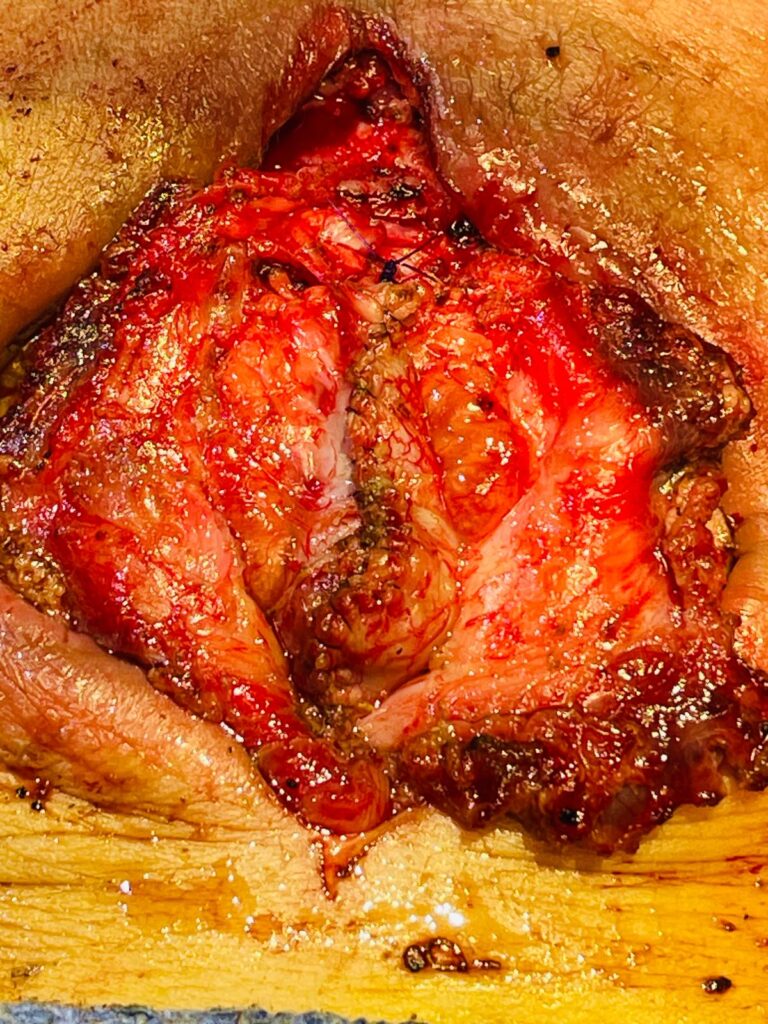
The next woman is HIV positive and has had abscesses all over her chin and neck from tooth decay and infections. She has a remaining hole just above her sternum that when she coughs or lifts something- pus drains down her chest from the hole. I decided this must be a retrosternal collection. So I numb her up and open the hole to probe it further. I worry about wether the internal jugular vein has been pulled or displaced by scar tissue- will I get into significant bleeding that is difficult to manage. I open a small amount at a time. I probe the pocket with an instrument and feel that it’s not to big. I had hoped to get my finger in, but I stop as Im not in bleeding and down want to cause it. I put a piece of glove in as a drain and put a dressing.
There are not many cases scheduled on the weekend so we are done. I head over to another missionaries house about 10 min drive away on a motorcycle. Unfortunately and fortunately they are just ready to have a late lunch. So we are invited to eat. We have a nice meal together and I spray the areas of their house they want sprayed with the insecticide I brought.
Back at the hospital I make it back in time to be a part of a party for one of the Cameroon missionaries here. Two of the families here made cake- and they taste real good! We take turns commenting on how we appreciate the person who’s birthday it is. It think this is a nice way to party.
Just at the end of the party there is a call for a woman who isn’t progressing in labor and has a face presentation. Normally the back of the head is the presentation part an this comes out easier. The face is to broad and doesn’t deform like the rest of the head for a vaginal delivery. We wait for the generator people to put in fuel as the power just went out. Then she starts bleeding vaginally. Now it’s an emergent C-section. We pour in the fluids and get a spinal in the dark by headlamp. We can’t wait for the power to come back on. We must get the baby out as soon as possible. She may have placental abruption (separation of placenta from uterus that will kill baby and make mom hemorrhage a lot). As soon as the spinal has taken effect quickly cut into the abdomen, down to the fascia. A quick cut and scissor of the fascia and separation from the rectus muscle. Move the bladder down out of the way then open the uterus. I immediately get some clots. I reach in and fish the baby out. He looks weak but starts little breaths. The midwife is there to receive the baby and she takes her, and starts working to get the baby breathing well. I close the uterus as fast as possible to help staunch the flow of blood mom is loosing. Then tie off some other bleeders. Mom is getting a transfusion at the same time. God help this mom and baby! I hear the baby start to cry- what a joyous sound!. The power flickers back on for about 1 minute then fades out again. Sweat is pouring in rivulets down my back and legs. I slowly close up the different layers irrigating between each layer. Mom has stabilized with more blood and all I feel now that my adrenaline is less- is HOT!! After we are done and wheel the patient to maternity, the slight breeze outside is sooo refreshing. The power takes a while to come back on. More plastic bag in the generator fuel lines I hear. Eventually the power comes back on and I’m able to sleep. Till 2AM when I’m called again.