Bere 5/2025 #12
Sabbath has been very hot. I thought it may rain today as it felt humid, but it didn’t. We went to the sacred forest this morning to look for whatever was living there. We found some little red bugs, a host of ants eating a dead lizard, and some different plants. We went to church and I sat with the missionaries doing the Childrens songs and sabbath school story. We had a church service that I translated to the medical student that came this week, as he didn’t speak French. Then on to my favorite meal here, potluck after church. All the missionaries get together and bring a wide variety of dishes. Indian rice, a boiled leafy dish, some dense meat like substance made form pumpkin seeds, white been fried blobs with a very nice hot sauce on the side, cabbage salad kind of like coleslaw, and mango cobbler for dessert. The company and the food were excellent. A visiting OB/GYN came today. Great for Dr. Staci who is always overworked with OB being only one of the many things she does. After potluck I went in to see a comatose man who came that way yesterday. He has a liver tumor or abscess. Ultrasound wasn’t clear. His BP is low, so I ask the nurse to give more saline. I get back to the group and the nurse calls again. Another patient is also in a coma and isn’t breathing well. I go to check on them. I see they are being treated for malaria. Family says at noon she was talking. So I imagine Quinine has dropped her blood sugar. Her glucose is 71, low. So I ask the nurse to start glucose right away and to call me if she doesn’t wake up soon. A group is going out to the monkey forest so I join them. We drive about 20 minutes and then walk into the forest on a very small path. We get to a place where there are large trees with a lot of under brush, and vines are growing on the trees. They said when they’ve been there before the monkeys get curious and come to check them out. We wait for 30 minutes then give up. A guy walking by says that the forest is about 2km in a direction. I had no idea it was that large. Morning about 6-7 is best he says. On the way back I get a call from the ER saying there is a guy with a bowel obstruction for 2 days.
I walk to the ER and see a 60 year old man laying on a mat with a round belly and a foot propped up on a bench. He is grunting in obvious pain. He says he hasn’t pooped in 10 days. Wait I thought 2? No 10 days of no BM, vomiting and feeling awful. The guy is very thin with a taught belly. He doesn’t seem to have peritoneal signs. So what will I find with my digital CT. (using my digits to Cut and Touch :)) I try to call Phillipe- no answer. I try to call David- no answer. A radiology nurse is just leaving so the ER nurse asked him to go by Phillip’s house to get him to come in. I ask her to call me when he gets there. In about 30 more minutes he’s there.
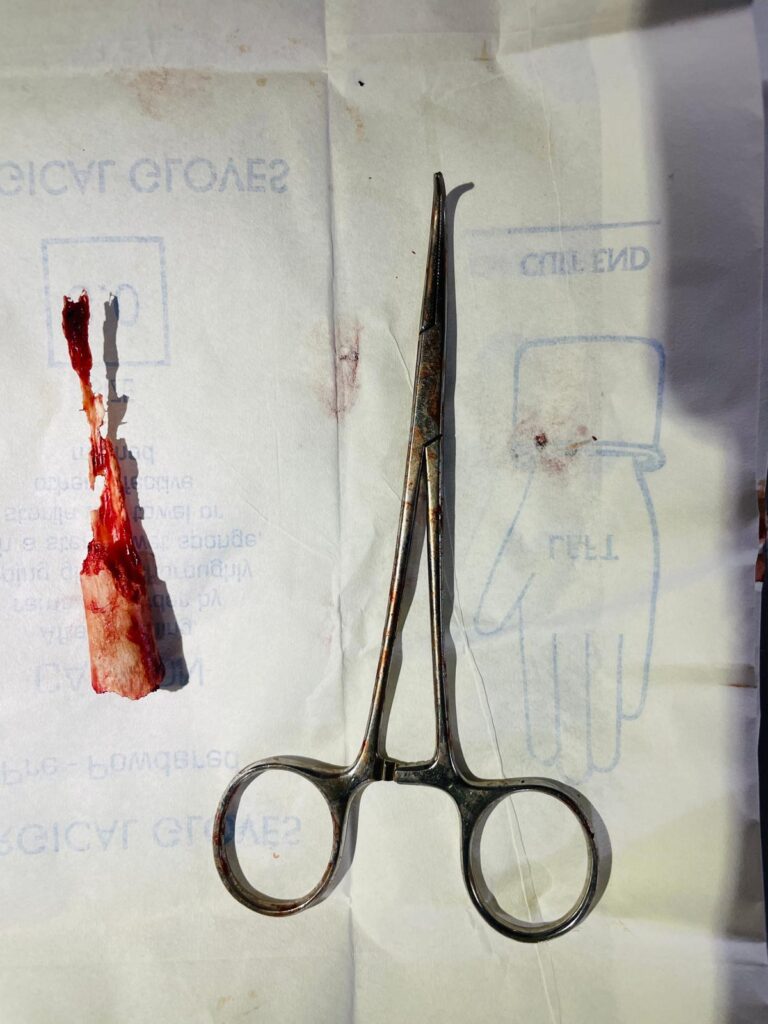
In the OR Phillipe prepares for general anesthesia. I choose the OR pack wrapped in cloth that I think is an exploration pack. I choose the suture, gloves, covering for the bovie cord, and suction tubing also wrapped in cloth. I try to find the one that feels like the silicone tubing I brought last year as it makes it through the autoclave better. The med student Caleb puts in a foley catheter and I prep the patients abdomen with Betadine. Philippe intubates this patient without any problem. I scrub at the sink with the bar of brown soap and then put on my cloth gown, then gloves. There is an under apron I could put on to keep the patient fluids from soaking through to my skin, but Im so hot already and sweats running off me, that I don’t want to add heat to what Im doing. I slice open the skin with a few swipes. The skin is tough and the non-US scalpel isn’t very sharp. I go through the layers and when I get a small hole into the abdomen pus flows out. Really? He didn’t have peritonitis on my exam. So obviously he’s really tough and didn’t demonstrate the pain he was in. Pain he has been in for at least 10 days. I don’t know where he’s from, but the travel here must have been terrible. We suck 2 liters of pus out of his abdomen. Then the search is on to find the source. I think it must be the stomach or appendix. As I feel around more loops of bowel separate and more pus comes up. The right lower quadrant seems a bit stuck and firm. I search for the appendix and find it necrotic with an appendicolith in the abdomen. I try and get out all the necrotic stuff I can, including the appendicolith. I tie off the base of the appendix and take the offending organ out. I run the small intestine through it’s length looking for any injuries I may have caused getting the adhesions to release and there is a spot likely effected by typhoid but nothing is thin in the wall so I leave it alone. We wash out the abdomen with many bottles of saline. Then we close the abdomen. I close the skin loosely allowing for a wound infection to drain out.
As Caleb cleans up the room and Phillipe extubates the patient, I sit off to the side and write my op note and write orders for his post-op antibiotics and his Diclofinac pain med. I’m still waiting for the extubation so I get some scissors that I’ve been trying to sharpen and start working on sharpening them. Something bounds towards me on the floor, I reflexively KICK, and a rat is hurled across the OR and scurries back under and into the rack of urine catheters and all the other OR stuff in the room. I can’t believe a rat just ran towards me. Well it was very surprising and then again, of course there must be rats, they’re in peoples houses and missionary houses, so why not the OR. I will try to get a rat trap from somewhere to help that not occur again! After extubation I head home at 11PM to try to wind down and sleep.